You are currently browsing the category archive for the ‘Real life’ category.
Eleven years ago on Mother’s Day, my friend Kerry started something on her socials. Kerry’s mum sadly died when Kerry was just six years old. She doesn’t have a single clear photo of the two of them together. And so, Kerry has urged her mum friends to make sure they take a photo with their kids – a really simple and special way to make sure that memories are recorded. (You can search for #KTPhotoForMum to see some lovely shared posts.)
We’re not short of photos in our household – who is in the age of smart phones? – but I especially love the album that I have of Mother’s Day photos of me and our girl. Seeing her on this day for the last eleven years brings a special feeling of joy.
But there’s another feeling in there that I want to recognise, and that’s how proud I am. Of course I’m proud of her – she’s a marvel (excuse my bias). But I’m talking about hoe I feel about myself as a mother living with diabetes. Because pregnancy and parenting with diabetes is not an easy gig.
I struggle with this sometimes. I don’t want to be defined by being someone’s mum. I achieved a lot before I became a mother and have done plenty in the last (almost) 20 years that I am so very proud of. There’s travel and a career, and media work, lots of published writing and a whole lot of standing on stages talking diabetes advocacy. These are usually the things that I point to when thinking about my achievements. For some reason, I’ve felt it’s diminishing to point to motherhood as an achievement.
But the truth is, that motherhood with diabetes is an achievement and it is defining in some ways. Conceiving, growing a baby, bringing her into this world, and getting her to adulthood is something that carries a huge sense of pride. Because, damn, diabetes made that hard. Every stage of it.
I get it: pregnancy is natural and it’s been happening forever and there are bazillions of people who have done it for a bazillion years, but there is absolutely nothing natural about taking on the role of a human organ. Seriously! It’s hard at the best of times. Being pregnant adds a degree of difficulty that is incomprehensible until you’re in the midst of it. Even today with tools that are far more sophisticated than the basic pump that saw me through my pregnancy, it’s still not easy. (And I utterly recognise how lucky I was at the time having a pump. The women sitting next to me at the Women’s Hospital diabetes & pregnancy clinic on Wednesday mornings who weren’t using a pump were real magicians.)
At that time I was just so in the weeds of dealing with all that came with a diabetes-complicated pregnancy that I never thought what an incredible job I was doing just getting through it. After all when was I meant to cheer myself for the remarkable effort? Was it before or after the 20+ finger prick checks I was doing each day? (CGM wasn’t around then.) Or alongside the complex calculations that I needed to complete before pre-bolusing the right amount of insulin at the exact right time? It certainly wouldn’t have been during the thirty percent of the day I was below target because in those moments, I was too busy worrying about starving my brain (and baby) of oxygen.
And then there was no time after she came along, because babies are all encompassing and take up every moment of the day. And diabetes can also be all encompassing and is incredibly demanding.
I had no time to be a cheerleader for myself because every single part of me was focused on making sure my baby’s elbows were growing properly, and stressing about how any out of range glucose level was harming her growing organs. Any spare brain bandwidth was taken up feeling guilty because I never felt I was doing enough. I felt that I was probably already failing my child. Even though her elbows are beautiful (and her organs seem fine), I still carry that guilt. Almost twenty years later.
These days, as more people with diabetes share their pregnancy and parenting stories, I DO cheer. Every time I hear about chaotic first trimester hypos, and managing glucose levels around second trimester cravings, and third trimester insulin-resistance frustrations, I know they deserve a loud ‘Hurrah!’ and so I cheer. Because look at these amazing people! Look at what they are doing – the work, the emotional rollercoaster, the determined effort they are putting in to keep themselves and their baby safe! Diabetes never plays nice, and for so many, pregnancy is the most difficult time in someone’s diabetes life.
Yesterday morning, I looked at our daughter as we had our Mother’s Day breakfast in the sunshine. Having her is the hardest thing I have ever done – the hardest, the most emotionally challenging, the scariest – but also the absolute best and I am so very proud that I did.
This post is dedicated to my dear friend Kati who I am cheering for every day!

Living with diabetes has made me acutely aware of the importance of screening. Eye screening, kidney screening, neuropathy screening, mental health screening – they’re all part and parcel of my diabetes care.
In my mind, screening is a non-negotiable because I live with a chronic health condition that refuses to stay in its lane, instead, spreading the love around. And by ‘love’ I mean ‘puts a heap of other things at risk’. Diabetes, the gift that keeps on giving.
Similarly, I’ve always (mostly) been on the ball on cervical screening. Regular Pap smears were booked in every two years. Cervical screening is different now. It’s done every five years (yay!) and is expected to protect almost a third more people from cervical cancer than the Pap smears of old (also yay!). AND there’s a DIY version for those who would prefer. I love it when progress makes unpleasant medical procedures slightly less unpleasant!
After last year’s BIG birthday, I knew that there would be more screening, and sure enough, almost before I’d blown out the last candle on my drawn-out birthday celebrations, both the Australian and Victoria Governments were sending me love letters to help me protect my health. The Australian Government’s bowel screening program came with a kit to do the screening at home. And the Victorian Government sent me a letter, urging me to make an appointment for a breast check.
Diligently, I did just that and had a mammogram at a local BreastScreen Victoria centre. That was about three weeks ago. I didn’t think about it again until I was about to board a long-haul flight home and opened an email asking me to come back for a follow up appointment. There were changes on my screening mammogram that needed to be investigated further. I had a fun 30-hour transit home imagining every possible catastrophic scenario (because: melodrama) and have spent the last week and a half oscillating between ignoring things and stressing over them.
And that brings me to today. This morning, I had my follow up appointment, and the short story is all is fine. (The very slightly less story is I had a 3D mammogram, my breasts contorted into expert-level origami configurations, and a million images taken to show that all is okay. Come back in two years.)
Walking back to the car, I took deep breaths, scolded my stupid brain for insisting on making things bigger and scarier than they ever need to be, and then reminding myself that I should be kinder because it’s not just this screening that was influencing how I felt.
I don’t know what it’s like to not live with a chronic health condition that places so many expectations for regular health checks and pressures on my mental health. Honestly, I wish I did. Because I know that the way that I am feeling – the anxiety, the stress, the worst-case-scenario obsessing – is so shaped by twenty-six years of living with diabetes. I can’t switch off these feelings or react differently. I can’t force myself to think of things through any other lens, because everything I see is through diabetes-coloured glasses.
This is the reality of living with diabetes. And it’s the legacy of scary images and campaigns and messaging that told me it was all inevitable. Of course I’m going to expect the worst because I heard that all for so very long. It wasn’t a giant leap for me to head straight to thinking the worst thing about a call back following a mammogram.
And so, because community is everything to me, as soon as I could I reached out to a friend who has had breast cancer. I needed to connect with someone with lived experience. Who better to try to talk through things? And the next person was a friend with diabetes who had recently had an experience that pretty much mirrored mine (and the same outcome). Of course I read everything I’d been sent from BreastScreen Victoria, but I needed to humanise the situation. And the only way I could do that was by speaking with people with lived experience, who could climb in beside me and wrap me up in a quilt of understanding and reality. Community really is everything. – whichever community it is.
WHILE WE’RE TALKING COMMUNITY…
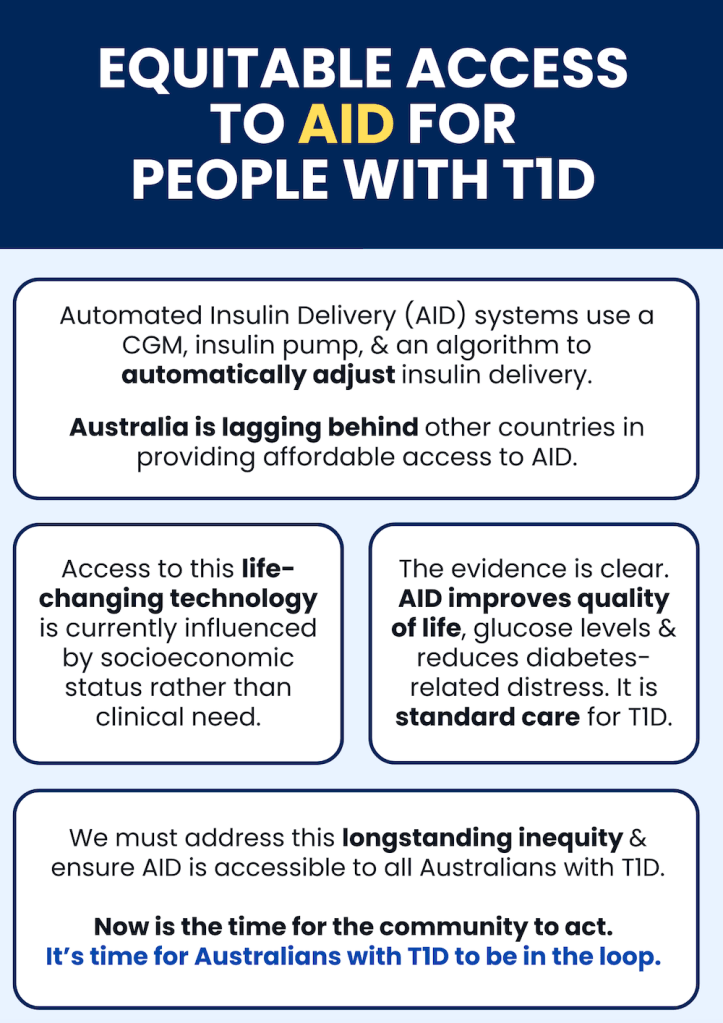
If you’ve not yet shared and signed the petition for equitable access to AID for Australians wth T1D, please do! This is a community-driven initiative, created by people with diabetes in consultation with other stakeholders who have come together to advance advocacy on this issue. It’s getting close to 1,500 signatures already, and I’m seeing it shared widely in community groups and organisations. Thanks to everyone who has supported the community by being part of this advocacy.
‘Why would you bet against the type 1 community?’ That was a question asked in a session at the ISPAD conference a couple years ago. It wasn’t someone with T1D drawing attention to the community. Instead, it was said by someone working in global health who had seen the remarkable efforts such as the #WeAreNotWaiting movement and grassroots, peer-led education initiatives in low-income countries. These efforts have driven change and improved lives of people with diabetes. They have been led by those with lived experience and supported by other diabetes stakeholders. But the starting point is people directly affected by diabetes identifying a problem, solving it and leading the way. In the history of diabetes – from the first home glucose meters, to building systems leveraging off existing technologies, to global advocacy movements – community powered initiatives have been a driving force for change.
And so, here we are today, coming together once again to advocate for better equity and fairness for all people with type 1 diabetes, this time in Australia, and this time advancing access to automated insulin delivery devices (AID).
Insulin pump funding is broken. AID is standard care and yet far too many people are left unable to use the tech because of how pumps are funded in Australia. Right now, unless a person with T1D has the right level of private health insurance, or meets the criteria for the Insulin Pump Program, they must find the funding for an insulin pump. That needs to change.
We know how to do this in Australia. The reason that pump consumables are on the NDSS is thanks to community advocacy efforts back in the early 2000. And more recently massive community noise helped to get CGM onto the NDSS for all Australians. Of course, these wins worked because everyone was involved in advocacy: people with lived experience of diabetes, healthcare professionals and HCP professional groups, researchers, diabetes community groups and organisations and industry. What a lot of noise we can make when we’re singing from the same song sheet!
Right now, attentions are razor focused on improving access to automated insulin delivery systems because the evidence is clear: AID reduces diabetes distress, improves quality of life, and (for those who like numbers!), help with glucose levels. And as an added bonus for the bean counters – it’s a smart, cost-effective investment for our health system.
If AID is standard care, financial barriers preventing people from accessing it need to be eliminated.
And that’s where we would love your help.
Please sign and share the petition that has been started by Dr Ben Nash and supported by a group of people with T1D (including me). Petitions are a great way to get people talking and interested in a topic. It builds momentum and helps contribute to whole of community conversations. While we know the T1D community is already on board, we’ve now seen a number of HCPs, community groups and diabetes organisations share and promote the petition and are keen to get involved with broader advocacy efforts. That’s pretty cool!
Postscipt:
Understandably, there are questions about why this work is specific to T1D technology access. That’s a fair question and I think that our very own Bionic Wookiee provided an excellent explanation of that when he said this in a social media post earlier this week:
‘AID systems were developed for T1D (where they can track all the insulin going into the system without having to cope with the body’s variable insulin generation). So right now they mainly apply to T1D…
Expanding CGM and pump access to people with other forms of diabetes than just T1D is important for the future. Having wider access to AID for the T1D population will be a beach-head for that.‘
And in a conversation I had about this with UK diabetologist Partha Kar yesterday he cautions that there needs to be a starting point because the sheer numbers of diabetes can be daunting and tend to scare policy makers. He also points out that when it comes to outcome modifying interventions, technology is THE thing in T1D, whereas in other types of diabetes there are other options. I’ll add that those other options often have stronger evidence which is why they already have funding.
Anniversaries – diaversaries – are for remembering. And today, my twenty-sixth diaversary, I’ve remembered that diagnosis day, and a lot of what has happened since. I’ve had a sensor fail. I’ve also enjoyed doughnuts, coffee and sunshine, and an AID so smart it has cleaned up all my diabetes incompetence and delivered a day of 95% TIR. Measure for measure, it’s been a good day!
My life would be impossibly different today if diabetes hadn’t moved in all those years ago. So much of my life, and so many of the people in it, is because of diabetes. The utterly confused and terrified twenty-four year old woman who walked out of a GP appointment after a diagnosis of T1D would never have believed the turn my life would take after I fell head first, and completely accidentally, into a life of diabetes advocacy. She wouldn’t recognise who I am, or how I fill my days and the people alongside me, the never-ending decisions I am forced to make, or the ever increasing stamps in my passport. She wouldn’t understand the normal that is my every day. But in the same way, I don’t remember her normal. (And thanks to Effin’ Birds for so beautifully illustrating that for me…)
Diaversaries are for remembering, but they are also for looking forward. Advocacy features so overwhelmingly in my future (and my present – I’ve spent a day off today working on an Australian grassroots community campaign). And so does advocating beyond our borders with the global access work I am so honoured to do at JDRF. And that means looking forward to people with a shared vision for real community and community involvement in ways that are meaningful and impactful. When I think of the last twenty-six years, community and others with diabetes feature so strongly. Because community is everything.
But perhaps most of all, diaversaries are a good opportunity to be hopeful. Advocacy has shaped who I am and how I have lived with diabetes, but hope has too. It’s as much of a driving force as anything else, something I hold on to every single day. I’m hopeful that access to diabetes care, insulin and other meds and technology becomes more equitable and that the heavy burden of diabetes casts an ever-diminishing shadow.
I stumbled across a book the other day called Women Holding Things. The author and illustrator, Maira Kalman referred to it as ‘love song to those exhausted from holding everything’. It’s quite gorgeous, with beautiful illustrations of all the things women hold – both literally and figuratively.
And I thought about what people with diabetes hold and just how weary and drained the weight of carrying diabetes and all that comes with it can be. I can’t draw, but here are my words that highlight some of the things we hold. It’s a love letter to the strength people with diabetes have gained through holding things, even when we want nothing more than to put it all down.
We hold on because we have no other choice but to do so.
We hold bags carrying around diabetes supplies – right now as I wait to board a flight, I have a separate bag with nothing more than sensors and pumps and alcohol wipes and spares of everything. I will hold it through airports, as I climb on planes, on ground transfer to hotels, and around with me through every step of my journey, a constant companion in my travels.
We hold cups of coffee because sometimes it feels like the only thing that will get us through the day.
We hold a fear of the future and what it can be, a shadow that sometimes stretches longer than we’d like.
We hold emergency hypo snacks ready for those unexpected moments. Or expected… (see: airports).
We hold guilt for some ridiculous reason because we shouldn’t and it is heavy and we would be so much lighter if we could let it go. But it’s there. We hold it.
We hold hope so close to our hearts, trying to balance up the fear or at least make a dent in its weight.
We hold insulin bottles and glucose monitoring supplies and all the little things that are needed to be replacement pancreases.
We hold anxiety and worry, and at times, a quiet uncertainty about what the next day, the next week, the next year holds.
We hold our diabetes friends close because they understand without needing explanations, and we hope that by being there for them as they hold us close, somehow there is a magic law of reciprocity that means we’re all holding less a little less diabetes.
We hold other diabetes stakeholders to account when they fall short of our expectations or fail to understand the nuances of our lived experiences, or underestimate our expertise. Or when they unleash a campaign that instils more fear.
We hold a steady gaze at research to see what our future life with diabetes might hold.
And we hold onto the promises, even the five-more-years promise that we know is a joke, but perhaps, just perhaps if we hold onto it tightly it might, it just might come true.
We hold our heads high as we advocate for better care, more understanding, and greater awareness.
We hold bottles of cinnamon, not because we know it’s a cure, but because it tastes great in the apple cake we’re holding onto for afternoon tea.
For those of us who can remember a before time, we hold on to memories about what life was like before we had to hold onto and carry diabetes.
We hold the hands of those whose diagnosis came after ours because we’re so grateful to those who came before us and held our hands.
We hold the key to lived experience and with it, we hold a unique perspective that must be listened to. Because we hold onto the belief that #NothingAboutUsWithoutUs
We hold a wealth of knowledge that comes from being a world class expert in our diabetes.
We hold a firm grip on the reality of life with diabetes because if we let that slip the consequences are too great to imagine.
We hold an inner strength that often surprises even ourselves.
Sometimes we hold back nothing as we tell our stories and and advocate for what is right.
We hold the power to change perceptions, influence policy, and inspire others.
We hold our spirits high when we feel we’ve had a win because holding onto those small victories carries us on through times where we feel we’re dropping the ball.
We hold our loved ones close, sometimes to protect them, sometimes to draw strength from their support.
We hold the courage to face each day, each challenge, with a bravery we often don’t credit ourselves for.
We hold a steady pace, because we know that diabetes is a marathon, not a sprint.
We hold onto the belief that it will be okay, that we will be okay. Because otherwise, there is nothing at all to hold onto. And that…that is just too heavy to contemplate.

The day after I was diagnosed with diabetes, I found myself in floods of tears, sitting in the stairwell of the Diabetes Victoria offices on Collins Street in Melbourne. I’d fled there from the NDSS shop that was housed on level three after suddenly feeling overwhelmed at the boxes and boxes of curious looking diabetes supplies that were about to be sent home with me. I was slumped against the wall, the emotion of the last twenty-four hours catching up with me. Someone came down the stairs and stopped. She crouched down and quietly said. ‘Hi. Are you okay?’
I wasn’t. Of course I wasn’t. ‘Can I sit here for a minute?’ she asked and somehow, through the tears, I nodded.
As it turned out, she was a diabetes educator working at Diabetes Victoria. And she also had type 1 diabetes. She spoke, I listened. And listened and listened. It was the first time I heard another person with diabetes share her experiences. She told me she too felt overwhelmed at times. And, she told me that right now – so new to it all – it feels so big, and that is perfectly understandable. She assured me that it would feel less big. She told me about bits of her life with diabetes and while she didn’t make it sound like bowls of cherries and puppy dogs, she took away tiny bit of the diagnosis fear that punches you right in the heart. Her stories made no sense at the time, but, as my own diabetes story grew, bit by bit, I understood her experiences.
I continue to search for stories today. I share some of mine – the things I feel comfortable sharing. And sometimes the things that aren’t all that comfortable.
I’m eternally grateful to that diabetes educator I met on 16 April, 1998. I told her repeatedly that her kind reassurance was the only brightness in those dark couple of days. I’m grateful to every other person who has so generously shared their lived experience. I never take it for granted – especially the reliving the trauma of difficult times.
And so tell your story. Only if you want.
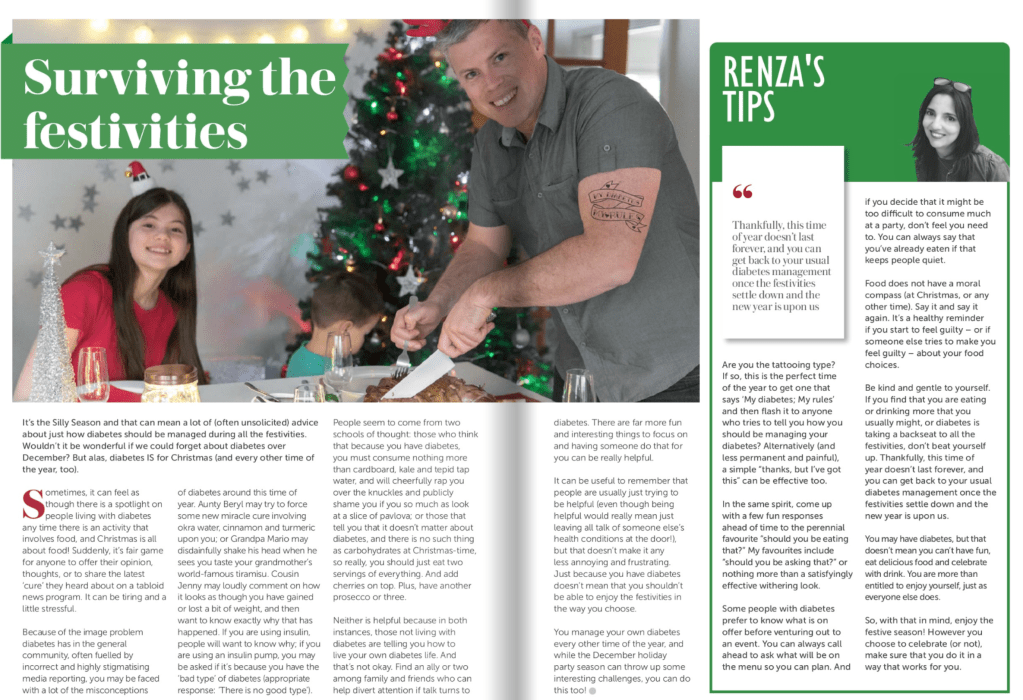
Do yourself a favour this Christmas and holiday period and do a detox. And by that, I mean cleanse and purge anything that suggests people with diabetes need to change our behaviour or feel guilty for daring to enjoy sharing a meal with family and friends.
There are a lot of those stories out there and annoyingly, social media algorithms keep pushing ‘How to be a responsible person with diabetes at Christmas’ articles to me. I wouldn’t be worried if being responsible included making sure I ate enough of my mum’s divine zippoli or kept the Bellinis flowing, but instead, it seems to be all about restricting portions and sipping flavourless drinks (water), and making sure I don’t throw diabetes or weight management plans out the window. Apparently, Christmas is as good a time as any to reinforce diet culture, demand food restriction and push punitive portion policing on PWD. Such tidings of comfort and joy!
People with diabetes have every right to celebrate festive meal without being made to feel judged or that our choices are being scrutinised. Our diabetes; our rules including what and how much we eat (or don’t eat). If I want to eat panettone for breakfast every day for the next month, it’s no one else’s business. What I don’t want is suggestions such as: ‘Overcome the urge for a candy cane, by brushing your teeth with peppermint toothpaste. Twice!’. Or ‘101 Ways to Enjoy Ice Chips: The Ultimate Low-Carb Snack’. Or ‘Chew on a cinnamon stick. It’s all the flavour of a spiced cookie without the enjoyment!’ Good tidings…unless you have diabetes.
Another theme that I see is the patronising reassurance that it’s okay for people with diabetes to ‘overindulge’. Cloaking assurances in passive aggressive pats on the head about how we’re allowed a ‘day off’ is unhelpful and perpetuates guilt. How about instead we accept and recognise that people (ALL people!) may eat more when celebrations are centred around food, and normalise it rather than make us feel bad for doing what everyone else is doing?
If we must be forced to read articles about surviving the silly season, it would be great if there was some merriment in there. It is possible! I did it here. And also in the article I’m sharing below that I wrote for Circle Magazine a few years back. Just some authentic musings about real life with diabetes, embracing the season with comfort and joy.
Christmas Giving
Insulin for Life is once again running their Secret Santa campaign. All donations go to support the charities efforts in supporting people with diabetes in under-resourced counties. If you’re able to donate, please do so here.
I had a BIG birthday this week. It was lovely – spoilt by my gorgeous family and friends, a beautiful dinner, calls and messages and special deliveries from friends in far flung places. BIG birthdays are weird. There seems to be an expectation that we have BIG feelings about them. Some people have BIG negative feelings about them. Some people freak out. Some go through a crisis and suddenly feel as though they are facing their mortality. I haven’t felt any of those things, but people have been asking. And I’ve been at a bit of a loss as to how to respond.
I don’t feel bad about getting older. I like that the cliché about women giving fewer fucks about others’ opinions as they age has been true for me. I like that I’ve become more confident, and with that developed the ability to recognise a bout of imposter syndrome and swiftly dismiss it, knowing I’ve absolutely earned the seat at whichever table I am sitting. I like that I easily stare down and call out misogyny and have become better at identifying the misogynists who cloak their misogyny in faux allyship. I like that I have a group of strong, sassy, spectacular women around me and that we build each other up and celebrate each others’ triumphs. I like the respect my work receives, and I especially like that I now walk away from situations where that respect isn’t afforded.
The only one BIG feeling I have had is that ageing is such a privilege. I’ve felt that keenly this week as I’ve celebrated this BIG birthday. I’ve thought of friends who didn’t get to celebrate this BIG birthday for all sorts of devastating reasons, and of friends who have had some pretty serious medical emergencies of late. I flashed back to my darling sister being so, so unwell last year, noting that when it’s time for her next BIG birthday there will be fireworks to celebrate that she is with us. And I’ve thought about how if I’d been diagnosed with diabetes a few decades earlier, I may not be celebrating this week.
Diabetes has been a constant and unwelcome companion for over half my life now. I do have BIG feelings about that, none of them good. It entered my life and reshaped it in ways that I couldn’t have imagined, and even though my work – work that I love – is impossibly intertwined with my diabetes, I feel cheated that so much of my brainpower, my energy, my finances and mostly, my time has been sucked away by diabetes. I’ve never bought into the toxic positivity of diabetes superherodom, and flat out refuse to credit diabetes for the discipline and resilience I’ve been forced to adopt just to manage living. I get credit for that.
And I’ve thought this: Ageing is a privilege, but ageing with diabetes feels like a miracle, and believing that brings into sharp focus my diabetes brothers and sisters who might not get to celebrate BIG birthdays due to completely missed diagnoses, inadequate healthcare, or lack of access to drugs and technology. Over the last few years, we’ve heard more from our vast community about those experience and we need to hear more, and do more to help. And so, if I can be opportunistic on the occasion of my BIG birthday, an appeal to anyone reading. If you can, please make a donation to either Life for a Child or Insulin for Life; two charities doing so much to increase the chances of more BIG birthdays for people with diabetes in under-resourced countries. That seems like the best celebration possible.
My Time in Rage over the past few days has been high; very high. That’s not a typo, I mean Rage (with a capital R). Since I published a post about airport security screening, a dozen people have messaged me with their tales of systemic failures that have left them feeling pretty damn overwhelmed. This is in addition to the myriad conversations I’ve had over the last twelve months. The situations may differ, but the underlying theme is consistent – this is a system that is not working, and people with diabetes are left exposed.
As systems break down, PWD are forced to deal with confusion, uncertainty, and a glaring lack of support. This is not confined to one specific area. I may have written about airports on Friday, but it spans across various aspects of our diabetes lives. The consequence is PWD in the firing line.
I’m forever thinking about the labour borne by people living with diabetes and how systems increasingly shift care responsibilities. Not only are we burdened with intricate care coordination and management, but also, we’re left exposed when navigating through systemic failures. Diabetes necessitates that those of us who live with the condition shoulder most of the care, but that burden shouldn’t then be compounded by systems that fail us – whether it be airport security checkpoints, or in healthcare settings.
Even worse, we know decisions are made around us, or without our direct input and when we highlight how things are not working, we are met with defensiveness and excuses. Inconsistencies, confusion, and a lack of clear communication may all be the reasons that things don’t work, but they are problems that are not ours to solve. It is not our role to make sense of chaotic labyrinths. We should not be expected to decipher the complexities behind systemic failures. Our focus should be on managing our diabetes, living our lives, and not on mitigating the fallout from systems that are supposed to support us.
I know that it can be argued that there are better ways to deal with matters than getting all rage-y. I agree with that; it’s counterproductive and draining. High Time in Range is often accompanied by distress, and hampered efforts to do diabetes well. It’s counterproductive and it’s draining. But sometimes, it really is difficult to keep that rage in check, especially when I believe that people with diabetes are getting a rough deal.